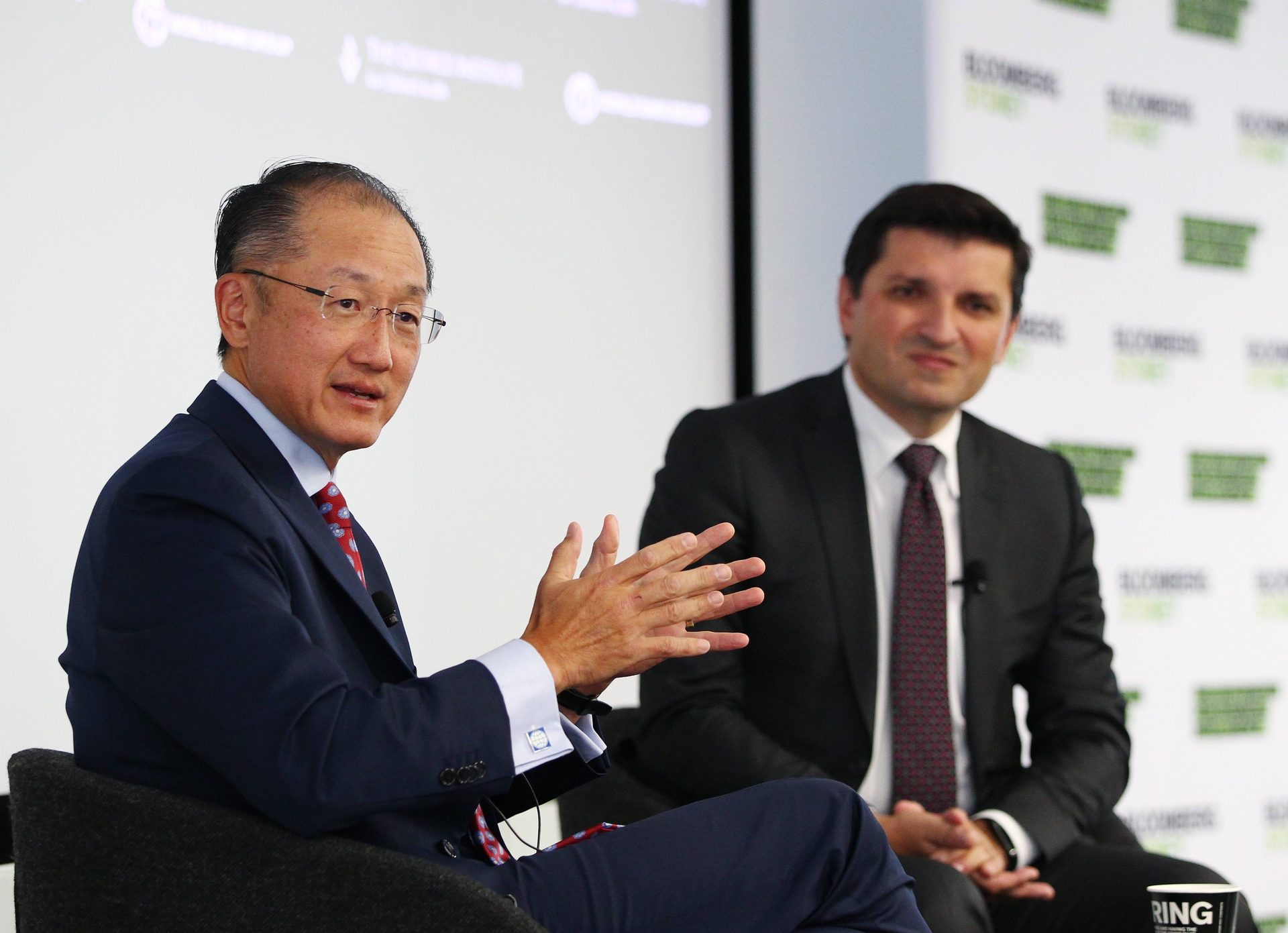
Transcript of Q and A between World Bank President Jim Yong Kim and George Institute Executive Director Vlado Perkovic
Jeffrey Leckstein Bloomberg:
We are delighted to welcome the World Bank and The George Institute today for this special event. On behalf of Bloomberg L.P, I would like to extend a warm welcome to President Kim who is in Sydney today ahead of his attendance at the G20 meeting [unclear]. I will now hand you over to the event moderator, Professor Vlado Perkovic, Executive Director of The George Institute for Global Health. Thank you. [Applause]
Vlado Perkovic:
Thank you very much. President Kim, distinguished guests, my name is Vlado Perkovic and it's my great honour to welcome you here today for this conversation with World Bank Group President, Jim Yong Kim.
Before we begin, I'd like to acknowledge the traditional custodians of the land on which we meet and gather, the people of the Eora Nation, and pay my respects to their elders, past and present.
We’d would also like to acknowledge the magnificent facilities and the kind generosities of Bloomberg L.P. for supporting this event on the eve of the G20.
President Kim, thank you very much for joining us. We're greatly honoured by you coming to talk to us today. As the president of the World Bank, you're at the very cutting edge of some of the toughest developments and economic challenges facing the world. You lead a global organisation that takes you to virtually every country in the world, and you have insights at a depth that's unusual, that we look forward to hearing a bit about today.
We don't have much time so we might get straight into some questions, if that's all right.
Firstly, you're here of course to attend the G20 Finance Minister meeting in Cairns. We've heard a lot about the growth agenda of the G20, but I'm sure we'd be keen to hear your take on the global economy today and the economic climate within which the G20 is operating.
Jim Yong Kim:
Well, first of all it's great to be here. It's actually my first visit to Australia, so I'm very thrilled to be here.
You know, It's another disappointing year. At one point our growth projections were as high as 3.2 per cent globally, and now they're around 2.7 per cent. So if you look across the world, the United States is doing well.
Growth seems to be continuing, and most of the numbers - employment numbers, et cetera - look pretty good. There are still lots of concerns in Europe, and I don't think we know the outcome of the Scottish referendum yet today.
But you know, there is some good news.
The southern European countries seem to be stabilising, but still there are lots of challenges.
I think there's concerns about deflation and there is a lot of uncertainty. Some of the uncertainty in Europe of course is related to the crisis in the Ukraine and Russia. And so far the impact of that crisis has been on the lower end of what our expectations are. But if it gets worse, if the tensions get worse, the impact could be much, much greater.
The Japanese have been making tremendous efforts to get back on the path of growth. Prime Minister Abe has shot his first two arrows and is attempting to shoot the third arrow, but we're still not sure. We're not sure if that third arrow in fact will land, and Japanese growth will get to where everyone is hoping. So there's still a lot of uncertainty.
A lot of middle-income countries, Brazil is slowing down.
China seems to be stable at about seven and a half per cent, and the good news in China is that while growth in China is still quite a bit lower than what they were used to, 10 per cent growth rates year-on-year, the leaders still seem to be very focused on the reforms.
So a disappointing year, but not a disastrous year.
In that context, we're very grateful to the Australian leaders for bringing the focus to growth. At this meeting what we're going to do is sit down and say, okay, if we want two per cent growth in the world, here are all the things that all the G20 members have to do to get there.
So that's what we'll talk about. We'll talk about whether - what the G20 members are doing and their specific efforts.
I think right now if you put all the efforts on the table, the IMF and OECD have suggested that we're at about 1.6 per cent growth.
So there's still more work to do, but I think the G20 has proven to be very useful to be a forum where we know that everyone's going to be held accountable. You have to come and you have to say what you're actually going to do. We're looking forward to hearing what the countries will bring to the table tomorrow.
Vlado Perkovic:
So the World Bank is a development institution, and its goal is to end extreme poverty around the world. What's your message to the G20? Do you think that growth will fix the poverty problem?
Jim Yong Kim:
Growth, if it leads to the creation of good jobs, especially for poor people, especially for women, especially for marginalised people, can have a huge impact on poverty.
The most extraordinary experience in lifting people out of poverty was China, and probably two-thirds, maybe even a little more than two-thirds of the success in lifting people out of poverty was just purely due to the growth of the economy.
But it's not enough.
We have two goals at the World Bank Group.
One is to end extreme poverty by 2030. But for the first time we're focusing on what we're calling shared prosperity. In other words we're tracking the income growth of the bottom 40 per cent of the developing countries.
This is the first time we've really looked at this question of inequality. I don’t think there's a single leader who doesn't want to have more inclusive growth, a prosperity that's shared by more people. I think everybody - every leader I've ever talked to tells me all the time, we want to grow the economy, but we want to do it in a way that more people can participate.
So there are all kinds of things that the governments can do, and the message that we'll send is investments in people are really important: health care, education, social protection programs. But also there are things that you can do even through your budgeting process, for example, that will lead toward greater gender equality.
So we're going to be constantly bringing up this notion of shared prosperity. And our role then is to bring to the table real experiences where governments have been able to shape the growth path, so that it was in fact more inclusive.
We believe that in everything you do, even when you think about how and where to build the road - building roads is really important, especially in developing countries. But if you can build roads that then give farmers, especially poor farmers, greater access to markets, then not only are you investing in essential infrastructure, but you're investing in essential infrastructure in a way that is bringing more people into the economy.
So that will always be our message. And I'm sure that we'll be having a lot of discussions about those issues around [inclusivity] and equity this time as well.
Vlado Perkovic:
So you've mentioned healthcare, which is of course the focus of the George Institute's activities. The biggest story at the moment is the Ebola crisis in Africa. A few weeks ago you wrote in The Washington Post that the Ebola crisis comes less from the virus itself and more from the deadly and misinformed biases that have led to a disastrously inadequate response. Strong words. It's a few weeks on now. How would you characterise the response today? Have we made any progress such that we're now equal to the challenge?
Jim Yong Kim:
I think the progress, even in the last few days, has been tremendous. The US commitment was extremely welcome, and I think it's going to be very helpful. Just as I was getting on the plane to come here, I was on a phone call with the Secretary General and many of the leaders of the UN agencies, and we talked about really pushing the envelope, meaning that there will be missions now.
So in other words, the Secretary General is handling Ebola as if it were sort of an outbreak of war, where instead of sending peacekeeping troupes, we're going to send in people who are going to be battling Ebola. I think the notion that it's going to go to the Security Council, that it's really a security threat, is also very helpful.
We found that during the AIDS - the early part of the AIDS epidemic when we were just beginning to think about treatment, That really helped, the Security Council taking on AIDS.
But you know, I think that at some point we're going to look back and have to ask this question: why did we wait so long?
Right now the focus has to be on getting the implementation, getting the people on board, getting the equipment, getting the drugs. You know, part of it was that I think people felt that being able to do management of electrolytes, being able to do intravenous hydration, that this was just too difficult.
It was very frustrating for me because I've spent most of my adult life trying to convince people that you can do very complicated things. We've been able to do things like drug-resistant TB treatment and HIV treatment.
And we have - in my own career and with Partners in Health, our role has been to say no, it's not too complicated. In fact you can do this very effectively using community health workers and nurses.
So I was a little surprised that that's again what we had to do.
We had to make the case that we've got to increase the complexity of our intervention, and if we do, we can really decrease the mortality rate.
At the World Bank Group they started asking some questions: what is going to be the impact of the Ebola crisis? What's going to be the impact economically?
When we looked at SARS and H1N1, what we found is that 80 to 90 per cent of the economic impact was not because of people who were sick with the virus. It was because of what we call the aversion behaviour as a result of fear around the virus. So in Liberia, Sierra Leone and Guinea as well, that's what we expect.
If we get treatment facilities in place, if we get infection control procedures in place that will cover the entire population, it almost doesn't matter how many people are infected. What matters is if our ability to treat and prevent is equal to the number of people who are there.
If we get that in place then what's going to happen is that people are not going to run away from authority anymore. People are going to be much more likely to go back to the fields, go back to the mines, get back to work. Then if we can get that to the point where the number of cases is not overrunning our ability to respond, then I think we can really eliminate almost 80 to 90 per cent of the economic impact.
But that means we have to move really quickly. I've been on the phone with teams in the field.
What does this mean? It means we've got to get things like oral rehydration to everybody. We've got to get intravenous IV hydration to just about everywhere, even in the villages. We've got to be able to monitor electrolytes. If we do that, we have no idea what the survival rate is.
The Ebola virus has never run into a modern, first world healthcare system. It's never happened.
Our own sense is that if you get those pretty fundamental basic things in place, that we can have a very high survival rate. If you have a high survival rate, if you're preventing new infections and you have enough in place for everyone, then the whole narrative around this disease changes.
We have a very small window to get that done. Our hope is that with all the efforts now, that we can do it in the next four to six months. If we don't do it in the next four to six months and it spreads to 15 countries and 22 countries, the impact could be absolutely incredible.
Vlado Perkovic:
A scary concept to think about. The human toll of Ebola is obviously absolutely terrible in the mortality and morbidity rates. What about the economic costs? What's your best estimate of the economic costs of Ebola?
Jim Yong Kim:
Just for 2014 to the end of the year, the three countries, Liberia, Sierra Leone and Guinea will lose about $360 million of their GDP, which is a significant amount because they're small economies.
But if you look at future impacts, if you look at 2015, if we get all the response in place so that we're preventing and we're treating everybody in those three countries, then the loss of GDP in 2015 is going to be around $90 million. But if we don’t get those in place, the loss of GDP is going to be over $800 million. It's a tenfold increase in the economic impact depending on how quickly we get those services in place. Again our hope is that we do it.
If we don't get those services in place and we start seeing outbreaks in neighbouring countries, in Nigeria and Ghana and Senegal, then the numbers could get very high, well into the many, many millions of dollars.
The great news is that there's this single intervention, getting treatment and prevention services in place, is the effective response to the contagion related to the virus, and it's also the effective response to the contagion related to the fear and aversion behaviour that happens if that treatment is not in place.
This is pretty simple. This is not about finding a new drug. It's very simple. You detect the cases. You prevent the infections.
This is not through some sort of space-age intervention. Any hospital in Australia could prevent the spread of Ebola as a matter of routine. It's universal precautions. Most of the hospitals in developed countries utilise universal precautions. If everyone used universal precautions, there would be no threat of Ebola.
So we just - the frustrating thing for me is that people who don't have experience doing clinical interventions in really poor settings, they walk in there wanting to be heroic and they see how complicated it is and they walk out saying it's not possible. That's what we have to stop. We have to stop having amateurs go in and say it's not possible because we know it is possible.
Right now, the good news is the US Government, the World Health Organisation, the UN, physicians whom I've worked with for years who have experience with these complex health interventions are working very closely together and are very close to coming out with a consensus approach that will bring all that complexity to the field.
Vlado Perkovic:
Africa seems a very long distance away from Australia, Ebola is a global issue that we need to deal with. So maybe can I get you to comment on the role Australia should be playing, and countries like Australia, in addressing the challenges imposed by Ebola.
Jim Yong Kim:
Well, I think it would be great if every country could see this as their own problem. One of the big, I think, reasons for the long delay is that people kept thinking of Ebola as an African problem or a Liberian problem. This is just - if we do that - for example if an influenza pandemic breaks out or if bird flu or if some form of coronavirus which was the virus that was responsible for SARS, I hope that we would react differently.
Everyone has to understand that Ebola is not something that's just limited to one region or an African problem; it's a human problem. I think that there's going to be a call for more money, we're going to need more money, more health personnel. I think it would be great for every country in the world to participate in some way.
Even more important though is that every country in the world, especially the developed countries, have to sit back and say okay, so how can we do this differently next time, because we're not going to have this kind of time if it's an influenza outbreak or if it's a much more quickly-moving airborne epidemic.
I think that we have to admit that there's a long way to go for us to be ready for a severe outbreak like that that can just move across the globe much, much more quickly.
Vlado Perkovic:
So moving to perhaps non-communicable diseases, just to change focus a little bit, and you're the first doctor and the first development professional to lead the World Bank Group. You talked earlier about the fact that most disease - the burden around Ebola could be addressed by simple health precautions. Of course, that's true for most non-communicable diseases at the moment as well. We have the challenge of providing care to those people who need it. What do you see as the biggest challenges in building a protocol for health systems around the world, particularly in countries, in our region here in the Asia Pacific area where the need is so great?
Jim Yong Kim:
I think first of all the most important thing is we have to really shift the way we think about investments in health care.
Twenty years ago when the World Bank and IMF were approaching their 50th anniversary I was part of a group that was protesting against the World Bank, it was called 50 years is enough and we made the argument that the World Bank should close its doors on its 50th anniversary. Our critique was mostly because we felt that the World Bank and IMF were not really focusing on things like health care. As a medical doctor working in global health, investments in health are almost an afterthought.
In a recent study that Larry Summers led, that was in The Lancet , showed that from 2000 to 2011, fully 24 per cent of the growth, economic growth, in developing countries was the result of better health outcomes.
So now I think there's a real understanding that investing in health is part of your economic growth strategy.
Now that we know that, then the question is then how do you do it? What do you invest in first; what do you invest in next? Every single country I visited, every single country I visited, they have - every single country in the world as far as I'm concerned - I have not seen one yet that's an exception - every single country has a problem with their health care system in some fundamental way.
So the poor countries have trouble just getting basic services, Sierra Leone and Liberia as an example of that.
If you go to the middle-income countries they almost all have the same problem, which is very high-tech very expensive care in the cities and then difficulty getting services to the outer regions. Then in - because in the cities they're trying to really copy the health care systems of the developed countries and they're very sophisticated urban dwellers, you can see what health care is like in the most advanced centres and that's what they want.
Then of course also in developed countries the costs are skyrocketing and in the United States where we spend 17 per cent of the US GDP on health care, the estimate is that between 30 per cent and 50 per cent of all health care expenditures are not only not helpful but harmful. This is a huge and difficult problem.
So at the World Bank Group we're now becoming very serious about helping every developing country, or any country in fact that asks us, to help improve their health care system. Getting the basic services in place is really important.
But making really tough decisions about how much you're going to spend on PET scanners and MRI machines for middle-income countries and how you're going to make sure that rural health care is actually in place.
My own experience over the last 25 years is that we have not really taken seriously what I've been calling the science of health care delivery. The delivery part is the real rocket science. Basic science of course has advanced; there's a lot more to do. Clinical science has also advanced; there's still a lot more to do, but we've done almost nothing in figuring out how to build the systems that will actually work.
So that's one of the things that we're really going to focus on and especially in the poorest countries. But I think the Ebola example has taught us that we are not prepared and especially in the poorest countries to deal with these pandemics.
Vlado Perkovic:
We've got a few minutes for some questions from the floor. There are a couple of microphones. I'll ask you to raise your hands and perhaps introduce yourself and tell us where you're from before you ask your question.
Brian Doolan:
Thank you very much. Thank you President Kim. My name is Brian Doolan; I'm from an organisation called the Fred Hollows Foundation. We focus on avoidable blindness.
Your approach, your background in health is a fantastic background here to hold your current position. I'm wondering about the question of cost effectiveness of interventions.
Some years ago the World Bank released a report which illustrated cataracts. The intervention around cataracts is one of the most cost effective health interventions. We recently worked with the George Institute to look at the cost impact, or the cost effectiveness of eye health interventions in Vietnam.
In fact, PricewaterhouseCoopers in Australia here recently released a report showing the return on investment for investing in eye health was a return of four to one conservatively estimated.
So I guess my question is where does cost effectiveness fit into the analysis that you bring when you're going to be advising countries as to where they spend their increasingly scarce health dollar? How does an organisation like ours, which has a growing body of literature showing cost effectiveness around avoidable blindness, get that into the mainstream of the global public health debate?
Jim Yong Kim:
Well, looking at cost effectiveness I think is important. But I would say that we still are not very good at using those kinds of studies to help shape health care systems.
There was NICE, the National Institute for Clinical Effectiveness in the UK that tried to really look at different interventions and then make some decisions about which ones the National Health Service would pay for and which ones they wouldn't pay for. That is inherently a very difficult exercise, especially in developed countries.
Let's take the example of eye health and let's take specifically the example of cataracts. I think one of the greatest medical institutions in the world is the Aravind Eye Institute. So I keep asking, so if - just to get a sense of the scale, Aravind does about 300,000 cataract surgeries a year and the UK health care system does about 600,000. That’s double. And the cost in the UK in a nationalised system to do 600,000 cataract surgeries is $2 billion.
The cost of Aravind to do 300 is half of that, is $17 million, and they're using a lot of that, as you well know, to pay for the cataract surgeries of very poor patients. So Aravind has figured out very specific things about how often you have to sterilise the entire - the operating suite and how quickly you can do things. So I think Aravind has shown us that if you apply a very rigorous approach to doing certain things like cataract surgery, you can bring the cost down so that it's cost effective almost anywhere.
The most interesting experience is that I went to China and there was a private sector group that was using the Aravind approach to clinical treatment of cataracts but then had borrowed from Japan, the kaizen, the continuous quality improvement model of running their business end. What they were able to do was based strictly on getting the public sector payments - these are payments that are coming from the Chinese Government, they were able to cut costs by 35 per cent, provide extremely high quality care, provide free care to the poor patients who couldn't afford any kind of care, and still make money.
So what I would say is that I think that the Aravind model shows us that we should be able to provide cataract surgeries just about anywhere.
The cost effectiveness is not a static thing because you can look at cost effectiveness based on the US system or you can look at cost effectiveness based on the Aravind system and the numbers are completely different.
What we're doing as the World Bank Group is we've reorganised ourselves so that our health care group is now going all over the world. We brought everybody that works on health care together into one group, and they're looking all over the world to try and find the greatest innovations that can lower the price and improve the outcome of all the different interventions that we take on board and I agree with you, I think eye care is a very important one.
So cost effectiveness is important but you can't do that analysis outside the context of knowing what and how well the price can go by looking for innovation everywhere.
Vlado Perkovic:
Any more questions here at the front?
Claire Spoors:
Hi. Thanks very much. I'm Claire Spoors from Oxfam. We very much welcome the World Bank's analysis that inequality is actually impeding growth along with other eminent bodies.
In the St Petersburg Communique there was a discussion of the need for inclusive growth but in the communiques by the finance ministers since then that term has been dropped.
I'm just wondering how much the issue of inequality and the need for inclusive growth is actually being discussed? Will we see that back in the language being used?
Also, how do you feel about developing countries being able to engage in the tax reform that's being led by the OECD and the G20 considering those low-income countries were not part of those groups? Thanks.
Jim Yong Kim:
I'm not sure what the language is. The language that's coming out of this G20 is the language that will come out eventually from the G20 leaders meet.
I'm not sure what it will actually say, but I can tell you that just about every country that I visit is concerned about inequality and it's huge.
I talk about Thomas Piketty's book all the time. It was a best-selling book in the United States and it was this dense 700-page tome that almost everyone bought and almost nobody read.
[Laughter]
Jim Yong Kim:
I think it's an indication of just how much people are thinking about the problem of inequality. The Occupy Wall Street movement, there's so many different movements that are addressing this question.
This is why we've put shared prosperity at the very top of our agenda. So I can assure you that we'll talk about it.
I have to say Oxfam, the work that you've done, I can't tell you how many times I've heard the quotation that 85 people in the world control as much resources as the bottom half of the global population. Things like this are helpful.
What our role though is that in everything we do, we have to put on the table approaches to building roads, building bridges, building health care systems, in how countries put their budgets together. We have to constantly be putting on the table options for making investments that will be more inclusive rather than less.
We know that there are really, really good examples. Examples that you never would expect that would have an impact on inequality.
For example, Austria has built into their budgeting ways of improving gender equality.
What we're trying to do - we call it the science of delivery. What we're trying to do is capture those examples where countries have done really innovative things to move toward greater equality and in putting this in front of governments.
At the end of the day the governments have to decide but my sense is that we're not going backwards and I'll tell you why.
When I went to one of the poorer areas of Uttar Pradesh in India, I saw poor women in these towns on their smartphones watching videos. Some of them were Korean soap operas.
The point is that people everywhere know how people everywhere else live and it's going to be more and more like that. So I think the demand for participation in the global economy's just going to get higher. As that happens, we feel, at the World Bank Group, we feel that it is our load to do everything we can to diffuse knowledge about things that are working and try to build in more fairness, more equity, more inclusion into global market capitalism.
One of the interesting things about [Deakin's] book is that he writes in the book on page 20 that the two forces that have traditionally led the world toward convergence have been the diffusion of knowledge and investment in the productivity and skills of people.
Well that's what we want. We want to be at the centre of that and to try to drive the world toward greater inclusion.
Vlado Perkovic:
A question over this side.
Michele Rumsey:
Hello, Michele Rumsey from the WHO Collaborating Centre at the University of Technology, Sydney. I just wondered really - I'm very excited to hear you talk about delivery and a focus for World Bank on delivery of health care.
One of the groups that we work with in the health workforce is nurses and midwives. I feel they've been the poor relation really in a lot of our discussions over the years and yet we single-handedly know that if we increase the education of midwives and increase the capacity of nursing midwifery, it would single-handedly improve the maternal and child's health rate from 75 countries that are still struggling.
Just really wondering if you could give a comment on your thoughts around nursing, midwifery, health workforce generally. Thank you.
Jim Yong Kim:
One of the things that we're really stressing in the Ebola response is that numerous precautions, monitoring of electrolytes, providing intravenous therapy and keeping people alive because these are self-limited infections if you can just keep people alive.
All of this can be done by health workers supervised by nurses and this is how we've done the most complicated treatments: HIV treatment, drug-resistant TB treatment, in all of our community-based responses have been done mostly by nurses.
What we've found is that nurses do much better at treating these kinds of complicated diseases because they're much more willing to follow protocols and doctors feel like they need to make it up.
(laughter)
This has been proven again and again and again that the more you can get health care focused on protocols that people will follow, the better the outcomes are.
I think that there's no question that the solution to the problem of access to health care is what we've called task shifting, that the things that the doctors do in some health systems should be moved to nurses.
Nurses should take a very much stronger leadership role, especially in developing country healthcare systems and that utilising community health workers is both a great employment program and also is tremendously helpful in improving outcomes. Because it's not - what we realise, for example in tuberculosis care, that having a health worker actually observe treatment, watch people take their pills, was the most important thing in improving outcomes. And HIV as well - what we found was that doing the same thing, having people from the community help you take your medicines every day was the most important thing in improving outcomes.
So in a time when people desperately need jobs, these are great jobs. Nurses can be central to the kind of leadership we need to really extend health care, the kind of health care that will really make people healthier.
I work very closely with a gentleman named Michael Porter at Harvard Business School and he's trying to introduce the notion of value. Value is just simply health outcomes over dollars spent. What happens is we get so focused on one aspect of the value chain, the intervention, the treatment, the diagnosis, but actually better health is a value chain that includes many, many things. One of the things which I do is in HIV care.
What are all the things you need to do to actually have a healthy person living with HIV at the end of the day? Most programs were not focusing on compliance, on actually people taking their medicines.
So we made the argument that if you invest more to health workers in ensuring that people are taking their medicines, you actually make the overall value of your treatment much, much higher.
I feel very strongly that we've ignored far too long the role of nurse midwives and nurses in global health. I agree with you in maternal mortality and in terms of childhood mortality and infant mortality. Nurses are really at the core.
Vlado Perkovic:
We've got time for one last question.
Lucy Hobgood-Brown:
Hello, I'm Lucy Hobgood-Brown and I work with - in the Democratic Republic of Congo.
I've been getting appeals every day from Congolese healthcare workers in the very area where Ebola has struck asking if there's any way that Australia or the United States can do anything to redirect some of the aid and people power towards the Ebola crisis there. It's been quite a challenge to do that and I wondered if you had any suggestions on how we might alert people that the Ebola crisis is not just in West Africa.
Jim Yong Kim:
I think you should keep saying it. You should keep saying it every day.
Right now we don't have an agreed-to consensus on what the clinical intervention will be. So MSF has done an incredibly heroic job and they have gotten their death rates down as low as 20 per cent but their intervention, they do exactly one laboratory test which is the [unclear] and they do really one intervention which is oral rehydration.
So for example, if you're in an MSF clinic and you're vomiting, it's very hard to take oral rehydration. So if you added to the fantastically effective and heroic MSF response, if you added IV hydration management of electrolytes, blood draws that would follow any number of studies, if you could do that then we think you could get the survival rates up very high.
What you need to do then is to have WHO say this is the clinical response. So in every hospital this is what's going to happen. In the rural areas you start with this and this but quickly move to get everything else in place.
Once they have that - those of you – there’s a lot of health people here, tuberculosis therapy was completely random and every doctor treated TB differently until we had DOTS. So we need a kind of DOTS for Ebola and once that's in place then we need to get it in place in all the countries in the surrounding areas.
I worry a lot about DRC because once you're in DRC and it starts spreading and if there's no access to good care, then anyone with a fever, the smart thing to do is to run away from authority and go somewhere else where you think you might get care. So If DRC gets involved and there's an outbreak in DRC, then all of a sudden East Africa's involved.
So we have to move. And I guarantee you people are thinking hard about what's happening in those countries.
But the first step is to convince the world that we have an approach that is up to the task clinically, that we can prevent the infections, that everyone agrees that this is the intervention, WHO puts their stamp of approval on it and then we go.
I think at that point we have to make sure that every single country in the region has access to that level and that quality of service.
Vlado Perkovic:
Before we finish up, maybe just one last locally relevant question. There's a lot of discussion at the moment here in Australia about the potential value of the Medical Research Future Fund. Could you share your thoughts on that?
Jim Yong Kim:
I understand that there are some complicated politics here…
[Laughter]
Jim Yong Kim:
…which I won't comment on but I'll say if you look at the history of investment in medical research in the United States, it didn't really happen to a great extent until about 1950. Many people think there's focus on basic science goes all the way back to the early 1900s. It's just not true. Most of medical education was not based on basic science. Then in the 1950s and '60s basic science started to grow but it was really President Clinton in the early '90s that made the huge investments in [unclear].
If you look at the investments that were made in the national institutes of health in the United States and then look at what it led to in terms of the creation of jobs, economic growth, opportunity for scientists to then move their findings into industry and then really literally grow the economy.
It was one of the best investments that we've ever made. So in a completely generic way, completely separate from whatever the local politics are, I think that Australia is a country that if it did invest more in medical research, it'd have a huge impact on the world.
And that investment could turn around and especially in the medium to long term have a very positive impact on economic growth in Australia.
That's been the experience in the United States and so I think it's - I don't think I'd say the same thing for the Central African Republic. It's probably not the top priority for them but for Australia, I think that there are great institutions of higher education here.
In my previous life, we had a very strong relationship with Bond University. And there are great universities here, there are great researchers. I think that it's quite reasonable to think about investment in medical research as part of your investment in the future economic growth of the nation.
Vlado Perkovic:
Thank you very much.


